
Heart Disease: these are lesser-known risk factors
Most people know that the risk factors for heart disease are high blood pressure, smoking, raised cholesterol and being overweight. However, many people who have a heart attack do not have any of these traditional risk factors. Research has suggested that conditions such as gout, psoriasis, inflammatory bowel disease and rheumatoid arthritis are also risk […]

Most people know that the risk factors for heart disease are high blood pressure, smoking, raised cholesterol and being overweight. However, many people who have a heart attack do not have any of these traditional risk factors.
Research has suggested that conditions such as gout, psoriasis, inflammatory bowel disease and rheumatoid arthritis are also risk factors for heart disease. What they have in common is chronic inflammation.
In fact, some researchers have begun to re-frame cardiovascular disease as a chronic inflammatory disease of the arteries. Scientists sometimes refer to this as the inflammatory hypothesis of atherosclerotic cardiovascular disease (ASCVD).
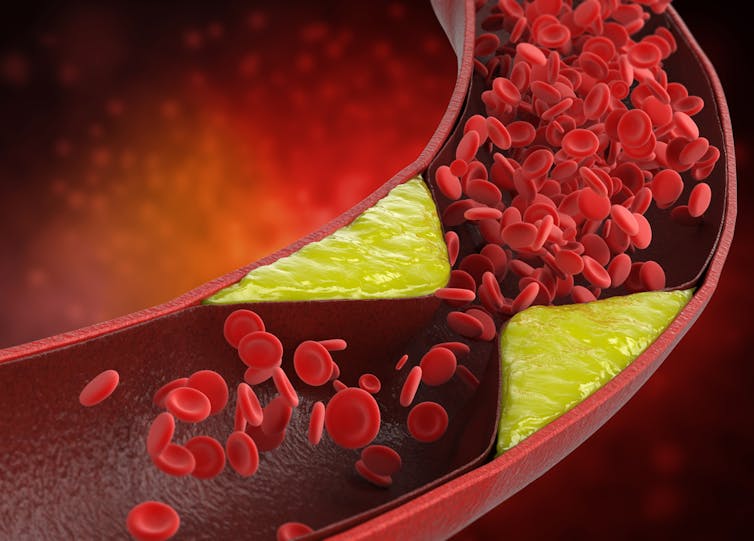
Atherosclerosis is where fatty plaques develop in the walls of our arteries, making them stiff. When this happens in the arteries that supply oxygenated blood to the heart, it is referred to as coronary artery disease.
ASCVD can cause heart attacks, where not enough blood is being supplied to the heart, and ischaemic strokes, where not enough blood is being supplied to the brain. To understand why ASCVD is an inflammatory condition, we need to consider how this process starts.
The first stage of developing atherosclerosis is thought to be some form of injury to the endothelium, the single layer of cells that line the arteries. This can be caused by high levels of low-density lipoprotein (LDL) cholesterol, sometimes referred to as “bad cholesterol”.
The toxins contained in cigarettes can also irritate the lining of the arteries and cause this initial injury. When the endothelial cells are injured, they release chemical messages that attract white blood cells, an important component of the immune system, to the site.
These white blood cells enter the artery wall and cause inflammation in the artery. The white blood cells also consume the cholesterol in the walls of the artery, leading to the formation of “fatty streaks” – one of the earliest visible signs of atherosclerosis.
Fatty streaks begin to form at a young age. By the time we are in our twenties, most of us will have some evidence of fatty streaks in our arteries.
This process of endothelial cell damage, white blood cell infiltration and chronic inflammation can continue silently over the years, eventually leading to the build up of plaque in the arteries. This may also explain why people who suffer from chronic inflammatory conditions are at an increased risk of cardiovascular disease.
Long-term inflammation of the arteries supplying the heart and brain can eventually lead to heart attacks and strokes.
A heart attack occurs when a plaque in the artery supplying the heart becomes unstable. This can lead to rupture (bursting) of the plaque, leading to a clot forming in the artery and the blood supply to the muscle of the heart being interrupted.
People who experience a heart attack often have increased levels of inflammation and plaque instability in the days and weeks before the event. The eventual “heart attack” and resultant damage to the heart muscle can be seen as this unstable inflammatory process reaching its zenith.
Because this chronic inflammatory process happens silently, many patients without traditional risk factors for heart disease will not be aware that they are at an increased risk of heart disease.
Measuring inflammation
Thankfully, there is a way to measure inflammation in the body. One way of doing this is with a blood test called high-sensitivity c-reactive protein (hs-CRP). People with raised levels of hs-CRP have an increased risk of heart attacks and strokes. Raised levels of LDL-cholesterol are also a risk factor for ASCVD.
Several studies have reported that people who have high levels of both LDL cholesterol and hs-CRP seem to have the highest risk of cardiovascular disease.
A large clinical trial called Cantos tested the inflammatory hypothesis of cardiovascular disease by treating patients who had had a heart attack and had high levels of hs-CRP with an anti-inflammatory drug called canakinumab.
The use of this anti-inflammatory drug reduced the levels of hs-CRP and resulted in a small but statistically significant reduction in the number of heart attacks experienced by these patients. Unfortunately, there also appeared to be an increased risk of infections in the group receiving the drug.
This risk, alongside the high cost of the drug, means it is not likely we are going to start using canakinumab to treat ASCVD any time soon.
However, the study was considered groundbreaking in that it supported the hypothesis that inflammation plays an important role in ASCVD, and that targeting inflammation may be useful to reduce the risk of repeat cardiovascular events.
Embracing this change in how we think about the risk factors for ASCVD may allow us to better identify patients who are at risk of heart attacks and strokes.
Also, this may enable us to focus on treating inflammation in order to reduce cardiovascular risk. Already, several studies are looking at using cheaper anti-inflammatory drugs, such as colchicine and methotrexate, to reduce inflammation and prevent the progression of cardiovascular disease.
Lifestyle changes to reduce inflammation
Fortunately, it is possible to reduce inflammation in our bodies without resorting to drugs. We can think of everything we do in our lives as being either pro-inflammatory or anti-inflammatory.
Smoking is pro-inflammatory as the toxins in cigarettes irritate the body. High levels of cholesterol in the blood and a diet rich in ultra-processed foods can also lead to chronic inflammation in our arteries. Conversely, a diet rich in fruit, vegetables, whole grains and fatty fish is thought to be anti-inflammatory.
Exercise also reduces the levels of inflammation in the body. Obesity, in particular carrying excess weight around your midsection, appears to cause chronic inflammation. Losing weight around your midsection will help to reduce this inflammation.
Stress can also induce a chronic low-grade inflammatory response in the body, and it is important to try to manage our stress levels. It is also important to maintain healthy blood pressure, cholesterol and body mass index – the traditional markers of heart disease risk.
By making anti-inflammatory choices and leading a healthy lifestyle we can all reduce our chances of developing heart disease and improve our quality of life.![]()
Robert Byrne, Chair Of Cardiovascular Research, RCSI University of Medicine and Health Sciences and JJ Coughlan, Researcher in Interventional Cardiology, RCSI University of Medicine and Health Sciences
This article is republished from The Conversation under a Creative Commons license. Read the original article.
